Governors have prioritized addressing healthcare workforce shortages related to retirement and burnout from the COVID-19 pandemic, the “silver wave” of baby boom generation workers aging out of the workforce and other compounding factors. To support state efforts to address these shortages, the National Governors Association Center for Best Practices (NGA Center) launched a Learning Collaborative to work with states on implementing strategies to strengthen and grow the next generation of the healthcare workforce.
The states in the Next Generation of the Healthcare Workforce project took a variety of policy approaches to address this challenge. Bringing project states together on this topic fostered discussion of best practices to address these challenges, and this paper summarizes these approaches and identifies best practices from the states’ efforts over the past year. Several themes emerged from this work, including the importance of:
While there is no single solution to solve healthcare workforce challenges, the policies the project states have employed have undoubtedly set them up for success and may be helpful for other states, territories and interested parties to consider. The remainder of this paper includes policy approaches organized thematically with state examples and conclusions summarizing high level project takeaways.
In recent years, Governors and state leaders have raised concerns over challenges related to recruiting and retaining the next generation of the healthcare workforce. A large percentage of the current healthcare workforce is nearing retirement age, which poses two unique challenges: hiring for positions left vacant by retiring personnel and filling the vacuum of knowledge and experience from these providers. With concerns over younger workers exiting the healthcare workforce at an early age due to trauma and stress related to the pandemic, filling these positions could pose an even bigger challenge for state leaders. Additionally, the American Association of Medical Colleges projects that the population of Americans over the age of 65 will increase by 42 percent over the next 15 years. Growing demand for the healthcare workforce to care for these older Americans places an additional strain on an already weakened system. On top of concerns over the rapidly aging healthcare workforce, the COVID-19 pandemic has placed additional stress on healthcare workers. With 20 percent of the healthcare workforce leaving the field since the start of the pandemic and an additional 20 percent contemplating leaving, concerns over staffing and increased workload create additional stress for healthcare workers. Additionally, nearly half of healthcare workers in a 2020 study reported feelings of burnout.
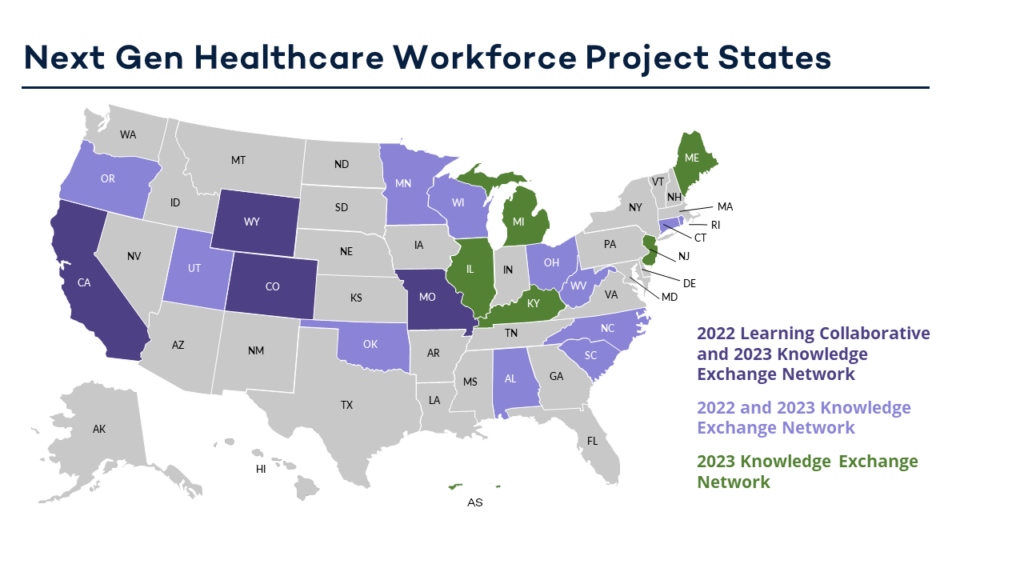
In response to this situation, the National Governors Association Center for Best Practices (NGA Center) launched the Next Generation of the Healthcare Workforce Learning Collaborative with support and funding from the U.S. Health Resources and Services Administration (HRSA). Starting with desk research and learning calls to understand the current landscape of the healthcare workforce, two NGA Center teams, the Healthcare Delivery and Postsecondary Education teams, came together to launch this project. In February 2022, the NGA Center released a request for applications for states interested in receiving technical assistance and support from the NGA Center through this project. In March 2022, the NGA Center announced that California, Colorado, Missouri and Wyoming were selected as the four Learning Collaborative States that would each assess their current operating environment, learn from national, state, and local experts, and develop and execute an action plan to achieve program and policy changes based on state-identified goals. In response to an overwhelming number of applications, the NGA Center decided to create a Knowledge Exchange Network to host an additional 12 states interested in supporting their healthcare workforce. The additional states received access to the healthcare workforce toolkit, received invitations to project webinars and joined the virtual kick-off meeting and in-person convening held with the full network group to share best practices. The Knowledge Exchange Network states included Alabama, Connecticut, Minnesota, North Carolina, Ohio, Oklahoma, Oregon, Rhode Island, South Carolina, Utah, West Virginia and Wisconsin.
NGA staff began the project by engaging in desk research and facilitating learning calls with experts in the field to gain a better understanding of the current landscape. NGA staff also engaged in learning calls with several states to determine the most important project goals for Governors and their staff members.
On April 27 and 28, 2022, the NGA Center hosted a virtual kick-off for both the Learning Collaborative and Knowledge Exchange Network States. The kickoff was attended by all four Learning Collaborative states, along with national experts and partners identified during the desk research and learning call phase of the project. The virtual kickoff featured sessions focused on the current healthcare workforce landscape, leveraging data, retention efforts, career pathways and professional development, resiliency and a first look at the newly piloted healthcare workforce toolkit. The kickoff featured speakers from the American Institutes for Research, the American Medical Association, the American Nurses Association, the American Psychological Association, Futuro Health and the University of Washington Center for Health Workforce Studies. Additionally, Learning Collaborative states had a chance to meet within their state teams to discuss goals with NGA staff and create an action plan for the project.
After the project kickoff, NGA staff continued to engage in research and hold learning calls to better understand the needs of Governors and their staff members as they work to recruit and retain the next generation of the healthcare workforce. During the first year of the project, NGA staff engaged in meetings with national experts and connected many of these experts to states in both the Learning Collaborative and the Knowledge Exchange Network through technical assistance and webinars.
The four Learning Collaborative states participated in monthly meetings facilitated by the NGA Center, consisting of goal setting, technical assistance (both intensive, goal-focused and supplemental), and action planning. Additionally, in partnership with consultants at Veritas Health Solutions, the NGA Center developed a limited-access healthcare workforce toolkit to support the participating Learning Collaborative and Knowledge Exchange Network states. This toolkit includes resources on topics such as mapping healthcare workforce stakeholders, understanding state licensing of healthcare professions and accessing data on the healthcare workforce; the toolkit continues to be developed based on state needs. Finally, to best support the full group of participating states, the NGA Center developed a webinar series that brought leading subject matter experts together with state project teams on a broad range of topics including diversity of the workforce, the nursing pipeline and healthcare career pathways. The Knowledge Exchange Network states also had access to the toolkit, as well as supplemental technical assistance and the webinar series, and contributed to vital peer-to-peer discussion on these topics as well.
To culminate the first phase of work, the NGA Center convened 12 of the 16 project states, including all four Learning Collaborative states, in Santa Barbara, California, in October 2022. The convening marked the end of the Learning Collaborative, with all four of the Learning Collaborative states providing in-depth report-outs on their work. Participants also heard recorded remarks from all four Governors of the Learning Collaborative states, California Governor Gavin Newsom, Colorado Governor Jared Polis, Missouri Governor Mike Parson and Wyoming Governor Mark Gordon, and each Governor spoke about his specific priorities and goals (for more details, see the Policy Approaches section on page 4). Additionally, participants engaged in topical discussions on specialized care, rural workforce challenges, industry collaboration and efforts to maintain momentum. States also had an opportunity to engage in peer-to-peer discussion to better understand the individual challenges and efforts of each state. With growing interest and continued challenges related to the healthcare workforce, the NGA Center announced at this convening that it would be creating a broad Knowledge Exchange Network of states participating in the project plus other states interested in joining to continue this important work through 2023.
This project supported states in preparing the next generation of the healthcare workforce by building on existing state programs and initiatives. The report includes both project outcomes from the NGA Center facilitated Learning Collaborative as well as the additional context on the states’ initiatives.
By working with Learning Collaborative states to set goals and develop an action plan, the NGA Center supported the advancement of state-specific strategies for specific workforce needs. Bringing project states together on this topic fostered discussion of best practices to address challenges. Several themes emerged from this work, including the importance of:
This section of the report outlines project outcomes from Learning Collaborative and Knowledge Exchange Network states and provides additional information on ongoing state healthcare workforce initiatives in each state to provide context for project outcomes and useful background or resources. The information on ongoing initiatives provides the context to understand more fully how states recruit and retain the healthcare workforce and how the NGA Center project states have built on these efforts.
Executive leadership and coordination across state agencies are crucial for developing and implementing a cohesive strategy to support the healthcare workforce. The Governors engaged in the project aimed to do this in a number of ways, including directing state project teams to focus on certain priorities, making budget requests, establishing councils, passing executive orders and working with the legislature to formalize and fund commissions. Cross-agency coordination is key as healthcare workforce issues touch multiple departments and communication across these groups can contribute to a holistic approach.
California: The California Fiscal Year 2023 state budget included a $1.52 billion investment in the healthcare workforce, driven by California Governor Gavin Newsom’s proposal in his budget. This investment aims to address workforce shortages as well as to increase diversity and linguistic and cultural competency in the healthcare workforce, requiring coordination between several agencies and stakeholders. As a result of working with the NGA Center, California developed a new position, Assistant Deputy Secretary of Healthcare Workforce, to support state healthcare workforce development in the Labor & Workforce Development Agency (LWDA). This role is tasked with building partnerships and strategic alignment across state agencies, healthcare systems, community organizations, and philanthropic groups for the state’s healthcare workforce initiative. California established the California Health Workforce Education and Training Council in 2022 in statute. The Council is tasked with planning education and training programs to support the healthcare workforce to meet the state’s needs. Council membership includes representation from the California Health & Human Services Agency (CalHHS) and the Labor & Workforce Development Agency (LWDA), community colleges and other higher education institutions, various health providers and professionals, and consumers. The Council tasks specific individuals with coordinating among agencies which had not previously had a formal way of coordinating. The group’s cross-organizational collaboration has supported connections to direct care and behavioral health workforce planning and funding, planning with community colleges and other educational institutions, employer cultivation and removing barriers to employment for justice-involved individuals.
Colorado: Colorado approached its healthcare workforce initiative through the framework of “Wildly Important Goals,” or WIGs. WIGs reflect Colorado Governor Jared Polis’ highest priorities for the state, and these goals are intended to bring more accountability and transparency to interagency work. Governor Polis’ Operations Team coordinates with state agencies to establish these goals, identify appropriate lead measures, operationalize new initiatives and track performance. Colorado launched a dashboard to visualize progress for these goals, one of which was to add 4,500 licensed direct care workers by June 30, 2023. The dashboard also illustrates agency-specific goals, like having the Department of Health Care Policy and Financing conduct a wage inventory for direct care providers to identify a livable, competitive hourly wage. This framework has increased cross-agency communication and centered progress on healthcare workforce initiatives.
Missouri: Missouri aligned its collaboration with the NGA Center with that of the Missouri Taskforce on Healthcare Workforce Development. This Taskforce coordinated across state agencies and other stakeholders to craft a report titled Strengthening the Workforce Pipeline: Recommendations for Public Health & Healthcare in Missouri which presents recommendations to address the future of the public health and healthcare workforce in Missouri. An outcome of this effort has been the establishment of the Public Health & Healthcare Workforce Advisory Taskforce. This taskforce is a working collaborative involving key healthcare entities from around the state. Leadership of the taskforce is provided by the Missouri Department of Health and Senior Services and the Office of Workforce Development. As a part of this state strategy, agency partners are developing career pathways and navigation supports to address critical access and retention issues for the healthcare workforce. Other taskforce recommendations include expanding access to middle school health science exploration programming, establishing incentives for expanded enrollment in healthcare and public health programs among other ways to increase opportunities to join and advance in the healthcare workforce. Specific state agencies are tasked with implementing each of these recommendations, making it clear which groups are accountable for achieving these goals and planning next steps.
Wyoming: Wyoming took a holistic approach to develop short- and long-term statewide healthcare workforce strategies by involving several state agencies and offices, industry and educational groups, and other partners. First, Wyoming’s state team included representation from the executive branch including the Office of Wyoming Governor Mark Gordon, the Department of Health, the Department of Workforce Services, and the Department of Education, a community college and the University of Wyoming. State legislators were also part of the workgroup and provided updates on the legislature’s upcoming bills to align healthcare workforce initiatives. In addition, Wyoming identified and invited several key external partners to engage in the work, including a representative from the Wyoming Medical Board. This team will continue to work together to coordinate efforts on key healthcare workforce education and clinical organization efforts as well as other related strategies to recruit healthcare workers to the state and stay in state in the future. Bringing these stakeholders together in a working group style format marks a significant step toward creating a plan that will touch many of the needs to address recruitment and retention of healthcare workers in the state.
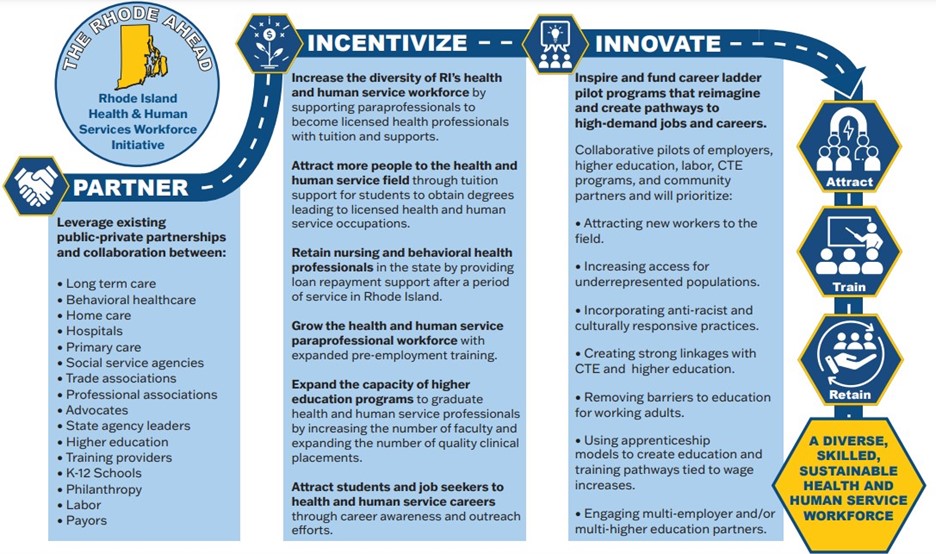
Rhode Island: In 2021, the NGA Center provided technical assistance to Rhode Island to help the state build a cross-agency coordination initiative centered on licensure data. Prior to that time, the state had numerous entities focused on specific aspects of healthcare workforce planning, but no single strategy for coordination across these initiatives. The Office of Health and Human Services and the Rhode Island Department of Health jointly requested assistance with this initiative. Information on state strategies for healthcare workforce coordination was customized by the NGA Center for presentation to state leaders and key stakeholders. On April 1, 2022, the Rhode Island Department of Health and Office of Health and Human Services co-hosted a Healthcare Workforce Summit, sponsored by the Rhode Island Foundation. The Summit was part of the states’ 2022-2023 Health & Human Services Workforce Planning and Implementation process. The purpose of this convening was to engage executive leaders in a strategic planning exercise to determine how Rhode Island might develop capacity for cross-agency health workforce coordination. Three principles guided the strategic planning discussion: building a robust and adaptive workforce, ensuring equitable workforce and workforce diversity, and improving systems sustainability.
Coming out of the Summit, Rhode Island established three informal workgroups assigned to investigate and produce recommendations with proposed metrics for prioritized areas: 1) Health & Human Services Pathways and Pipelines, 2) Health & Human Services Workforce Data Collection & Analytics, and 3) Health & Human Services Partnerships with Higher Education. NGA’s technical assistance to Rhode Island connected to the state team’s work in the first year of the Knowledge Exchange Network by providing a way to organize efforts and align stakeholders based on the state’s priorities. Although current workgroups are informal, meeting information (including presentations and minutes) is publicly posted. Rhode Island has since updated these workgroups to reflect 2023 priorities. These groups include Career Pathways, Pipelines, & Higher Education Partnerships and Workforce Data. A comprehensive progress report of Rhode Island’s health planning efforts was presented at the second annual Health & Human Services Summit in June 2023. A vision for the year ahead reflecting substantial stakeholder engagement, was also shared at the 2023 Summit.
Funding state healthcare workforce initiatives is an important aspect of these efforts. Many states have leveraged recent federal funds, including American Rescue Plan Act (ARPA) dollars, to support their initiatives. Finding long-term funding sources is important to make these efforts sustainable, and several states have incorporated their healthcare workforce goals into their budgets. Some states have also accessed philanthropic support and private funding through public-private partnerships to support these efforts.
California: California Governor Gavin Newsom dedicated $1.7 billion of the California Fiscal Year 2023 budget to healthcare workforce issues. After input from and negotiation with the state legislature, the final budget included $1.52 billion of mainly General Fund dollars to invest in healthcare workforce development. This includes $235 million over three years for new behavioral health programs such as expanding Master of Social Work programs and creating a psychiatry loan repayment program to support the state hospital psychiatry workforce. This funding also includes $281 million over three years to recruit, train and certify community health workers/promotors. Governor Newsom also dedicated $135 million for High Road Training Partnerships, training programs through community-based organizations, labor unions and employers to build career pathways for healthcare professionals as well as $130 million to create pathways into health careers for English Language Learners through the state’s Adult Education Consortia. Governor Newsom also invested $60 million to train opportunity youth for roles in Emergency Medical Services.
Colorado: Colorado Governor Jared Polis’ leadership was integral in securing the roughly $400 million included in Colorado’s FY22-23 budget for healthcare workforce initiatives. This includes over $280 million in ARPA resources to increase provider and direct care worker payments. The budget also includes $36.8 million for behavioral healthcare provider workforce development, planning, and education; $20 million to support the behavioral healthcare workforce through provider loan repayment and addiction counselor scholarships; and $15.2 million for department and community college behavioral healthcare workforce development activities. Governor Polis also invested in the Care Forward Colorado Program, which directs $26 million through HB23-1246 towards free entry-level certificate programs for healthcare workers such as certified nursing assistants, emergency medical technicians and pharmacy technicians. This program has since expanded through HB23-1246 to provide zero-cost credentials programs for in-demand jobs, including nursing, through community and technical colleges.
Missouri: Missouri used American Rescue Plan Act (ARPA) funding to support over $500 million in grants to higher education institutions through the Department of Higher Education and Workforce Development and $30 million in workforce training programs through the Department of Economic Development. The Missouri State Board of Nursing has awarded more than $13 million in grants for nursing education programs throughout the state to increase capacity and nursing education innovation. This includes nearly $3 million Missouri Governor Mike Parson approved in September 2022 through a special appropriation by the Missouri General Assembly.
Oklahoma: Oklahoma used ARPA funding to invest in the Health Care Workforce Training Commission, a state agency that typically provides scholarship funding to providers with a focus in rural areas. The agency was granted $96 million in ARPA funds that will be spent for numerous healthcare programs and projects across the state. These funds are being used to build new healthcare education buildings, renovate existing classrooms and labs, purchase medical equipment and supplies, provide scholarships to nursing students, and pay salaries for new and existing nursing instructors.
Wyoming: Wyoming used multiple sources of funding to support healthcare workforce initiatives. The state leveraged federal Coronavirus Aid, Relief, and Economic Security Act (CARES) and ARPA funding for nurse recruitment and retention efforts. This includes $7.5 million in ARPA funds for healthcare workforce staffing stabilization, such as retention and incentive payments. The legislature also approved additional funding for health and human service workforce issues in the most recent budget session.
Many states and territories are considering ways to ensure their healthcare workforce reflects the diversity of their populations. Research shows that a more racially and ethnically diverse workforce can support better patient use of healthcare through improved patient-clinician relationships as the workforce is more reflective of those seeking care. Gathering and analyzing workforce data is a key component of understanding state healthcare workforce diversity. The George Washington University Fitzhugh Mullan Institute for Health Workforce Equity developed and maintains a tracker to measure healthcare workforce diversity throughout the country. The tracker includes data on racial and ethnic diversity in ten health professions across states. Beyond data, states have employed certain healthcare workers skilled in cultural responsiveness.
California: California Governor Gavin Newsom’s goal is to recruit, train, hire and advance an ethnically and culturally inclusive health and human services workforce, with improved diversity, compensation and health equity outcomes. California’s approach to enhancing the diversity of its healthcare workforce includes investing in community health workers/promotores. Promotores share similar characteristics as the communities they serve and are primarily, but not exclusively, Latina women. These workers engage with Hispanic communities to connect individuals in need with health and social services, and the FY 2023 state budget includes $281.4 million over three years to develop this workforce. The California Department of Health Care Access and Information is currently working with stakeholders to develop training certification standards for these workers. California also launched an initiative to develop and support the diversity of the state’s behavioral health workforce. A total of $25 million will go toward strengthening the pipeline for this workforce with a focus on culturally diverse high school students. This program aims to increase access to important healthcare services for children, youth and families in the state.
Colorado: In 2022, Colorado Governor Jared Polis signed the International Medical Graduate Integrate Healthcare Workforce Act (HB22-1050) to better integrate foreign-trained medical professionals into the Colorado workforce. The Act establishes the International Medical Graduate (IMG) assistance program to provide technical support and guidance in this process, and the clinical readiness program to support skill-building for IMGs to join a residency program. These programs aim to leverage IMG training and enhance the diversity of Colorado’s healthcare workforce. While not part of the state team’s project work, Colorado also has an innovative initiative to advance cultural responsiveness in the healthcare workforce. The 2021 Colorado Health Access Survey by the Colorado Health Institute revealed that half of respondents reported feeling their provider “treated them with less respect or that their clinician was providing them with lower quality care than others.” The reasons given for this included financial status, race or ethnicity, disability status, gender identity and sexual orientation. This information solidified the state’s interest in developing a more diverse healthcare workforce. In 2022, Colorado launched the Colorado Option to promote affordable healthcare and culturally responsive provider networks. As part of the Colorado Option, state statute was amended to require standardized plans on the state-based marketplace to include a culturally responsive network that is diverse in terms of race, ethnicity, gender identity and sexual orientation to reflect the community served.
Oregon: Oregon collects and analyzes data on the diversity of its health care workforce. The Health Care Workforce Reporting Program has been in operation since 2009 and is part of the Oregon Health Authority (OHA). The program gathers data from 17 state health licensing boards from renewal surveys and produces insights to better understand the composition of the state’s healthcare workforce, inform policy recommendations, and steer educational and workforce investments. Oregon’s most recent report, The Diversity of Oregon’s Licensed Health Care Workforce, analyzes gender, race and ethnicity data to identify workforce trends over time. The report also includes data on languages spoken by the healthcare workforce, helping to inform the cultural responsiveness of providers and potential need for interpreters. The report is used by the OHA to guide strategies to help reach its ten-year goal to eliminate health inequities in Oregon by 2030.
In addition, the OHA also publishes reports that assess the health care workforce and its state-funded incentives and grants. Oregon’s Health Care Workforce Needs Assessment 2023 provides insights into workforce needs in communities across Oregon, expanding and diversifying the healthcare workforce, and distributing health care provider incentives. Evaluation of Effectiveness of Health Care Provider Incentive Programs in Oregon evaluates Oregon’s healthcare provider incentives and informs efforts to achieve health equity and increase access to culturally responsive care in urban and rural underserved areas of the state.
Understanding a state’s healthcare workforce supply and demand is crucial for determining how to allocate resources toward recruiting the next generation of these workers. States may gather this data from information collected and maintained as part of state regulatory processes, supplementary information on personal and professional characteristics, information collected as part of Medicaid provider enrollment or reimbursement and through a state data repository linking education data and workforce data. States are tackling this issue in a multitude of ways. Some states have created state-run research data centers explicitly for tracking their healthcare workforce.
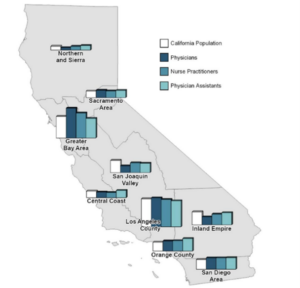
California: As part of NGA’s Learning Collaborative, the California state team connected with healthcare workforce data experts including Veritas Health Solutions and the Washington Sentinel Network. These connections contributed to the Labor and Workforce Development Agency partnering with the Healthforce Center at UCSF, supported through funding from the California Healthcare Foundation, to develop an evaluation framework for the state’s broader healthcare workforce initiative. In 2021, California elevated its Department of Health Care Access and Information (HCAI) from an office to a department through AB 133 which officially established the California Health Workforce Research Data Center (Research Data Center) within HCAI. The Research Data Center was created to serve as the state’s official source of health workforce data. As a result, beginning in 2023, all health licensing boards are required to collect core data element sets for health workforce analysis and provide this data to HCAI. The Research Data Center collects data on the current supply of healthcare workers, the geographical distribution of healthcare workers, the diversity of the healthcare workforce, the current and forecasted demand for healthcare workers and the educational capacity to produce trained, certified and licensed healthcare workers. All of this is also divided further by the specialty of the workers. With this data, the Research Data Center produces an annual report to the legislature that includes education and employment trends in the healthcare professions, the current supply and demand for healthcare workers in California and gaps in the educational pipeline producing workers in specific occupations and geographic areas, recommends state policy needed to address issues of workforce shortage and distribution, and describes the healthcare workforce program outcomes and effectiveness.
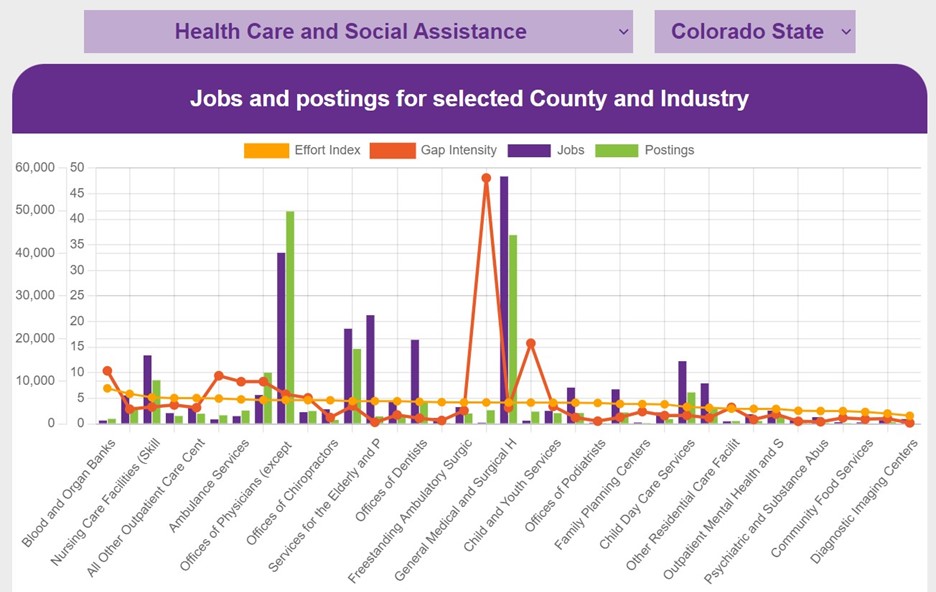
Colorado: The Colorado Governor’s Office collaborated with several state agencies and other stakeholders in a public/private partnership to produce the Colorado Future Jobs website. This resource includes charts and graphs summarizing the state’s employment demand by industry and occupation using data from Lightcast, the U.S. Bureau of Labor Statistics, and the Colorado Demographer’s Office. The Division of Prevention Services within the Colorado Department of Public Health & Environment monitors the collection and proper use of data in the state. The division assesses the healthcare workforce in both its rural and urban communities to determine where there are shortages of health professionals. It splits its data into four areas: a health systems directory which provides comprehensive data on licensed clinicians and healthcare sites, shortage area maps which provide data to determine if a specific community is located in an area of healthcare shortage, information on how a shortage designation can be used and how a community affected can apply to receive a federal shortage designation, and a workforce development strategy which can be used by communities or the state at large to strengthen the healthcare workforce. The Colorado team also created a tool to map state-designated healthcare provider shortages across the state. The Department of Public Health & Environment mapped substance use disorder and primary care health professional shortages as well.
Wyoming. Wyoming conducted a review of state healthcare workforce needs, data sources, and a landscape assessment to inform short- and long-term planning strategies as part of their action planning process. The aim was to identify data sources to help set state healthcare workforce activities. The team also assessed best and promising practices for critical workforce needs in the state which was critical to defining barriers and gaps in addressing the highest need workforce areas and supporting the development of educational and training program needs.
Rhode Island. In 2021, the NGA Center worked with Rhode Island to build a cross-agency coordination initiative. The Rhode Island Executive Office of Health and Human Services co-hosted a Healthcare Workforce Summit on April 1, 2022, to engage executive leaders in a strategic planning exercise to determine how the state might develop capacity for cross-agency healthcare workforce coordination. Coming out of the Summit, Rhode Island established three informal workgroups assigned to investigate and produce recommendations with proposed metrics for prioritized areas, including on workforce data collection and analytics. Although current workgroups are informal, meeting information, including presentations and minutes, from the Health & Human Services Workforce Data Collection & Analytics workgroup are publicly posted. This workgroup’s current focus is to identify what health workforce supply, pipeline and demand data elements may be available now and identify those that may be achievable with investments in data. For instance, during NGA’s project, the workgroup began developing a vacancy survey to understand hiring plans over the next six months, types of settings in which employees work, and current and budgeted vacancies for both full-time and part-time positions.
States focused on building out the talent pipeline for their healthcare sector have leveraged the career pathway development continuum. The federal Workforce Innovation and Opportunity Act (WIOA) includes a definition and overarching framework for the implementation of career pathways at federal, state, local and tribal levels. WIOA defines a career pathway as “a combination of rigorous and high-quality education, training, and other services” aligning with needed industry skills and supporting an individual’s career advancement, among other considerations. This definition is applicable not only to WIOA-eligible training programs but also to Perkins Career and Technical Education (CTE) programs. Some key elements of developing state career pathway strategies are to map the continuum of talent development in the secondary and postsecondary systems, including initial career exposure, work-based learning opportunities and apprenticeship opportunities. Colorado created a step-by-step guide for the development of industry-driven career pathways which includes strategies for engaging businesses, developing skills-focused training, marketing job opportunities and creating continuous improvement plans. The development of career pathways is reliant upon an analysis of industry needs and mapping of relevant education and training opportunities, and the state of Wyoming has developed a dashboard that collects, analyzes, and publishes timely and accurate labor market information that meet established statistical standards. Studying data from entities such as the U.S. Bureau of Labor Statistics and the U.S. Employment & Training Administration, the Wyoming Department of Workforce Services’ Research and Planning uses research and statistical methods to develop tools which provide analysis of the existing labor market. They cover a wide range of issue areas, including the health sector.
California: Under California Governor Gavin Newsom’s direction, the FY 2023 budget made several investments in the state’s healthcare career pipeline. This funding included $135 million toward High Road Training Partnerships for training and career advancement programs for people with barriers to employment, as well as incumbent workers. Funding supports collaborations and training programs among community-based organizations, local workforce boards, labor unions, educational institutions, and employers to build partnerships and pathways into family-sustaining healthcare jobs. Funding also went toward the Healthcare Workforce Advancement Fund for job entry and career advancement for entry-level and other workers in health and human service settings, through the State’s Employment Training Panel, with performance-based contracting that links payment to increases in wages for training participants.
Colorado: Through ARPA funding, the Colorado Department of Health Care Policy & Financing developed a project to strengthen their healthcare workforce and enhance rural sustainability. The department launched eight projects between October of 2021 and July of 2022 to mitigate the effects of the COVID-19 pandemic on the already strained sector. One of these initiatives is focused on career pathways. The department established income-based, affordable pathways to build career advancement opportunities for the healthcare workforce. Through partnerships with the Colorado Community College System, the Department of Higher Education and the Department of Labor and Employment, the state is creating more career development pathways for direct care workers. Through SB23-205, Colorado is establishing the Universal Scholarship program where all 2024 high school graduates and completers are eligible to receive a scholarship for education and training beyond high school.
Missouri: The Missouri Department of Higher Education & Workforce Development and the Missouri Economic Research & Information Center partnered to define in-state healthcare science and services career pathways. The state’s career pathways document (see Figure 3 for a section of this document) outlines the skills needed for different types of healthcare jobs. Career options are defined as requiring short-term on-the-job training, moderate- to long-term on-the-job training, or a bachelor’s or advanced degree, showing how jobseekers can advance from one role to the next with additional training. The career pathways document sources data from Burning Glass Technologies (which collects employer demand data), Competency Model Clearinghouse (which collects data on required job skills and training) and the U.S. Bureau of Labor Statistics (which collects industry wage data) to share entry and average wages for each role.
Wyoming: As part of the project action planning, Wyoming determined they would focus on building upon existing educational resources, training programs, and pathways in the state and in the region with neighboring states in the western part of the United States. The project team aimed to identify and develop educational and training programs that could meet their identified needs (e.g., apprenticeships, mentorships, degree programs, certificate programs) and understand best practices for credentialing and clinical training to retain healthcare workers or create new opportunities for additional training programs. The team also put together a plan to develop financial support programs to complement existing loan repayment recruitment and education financing programs. The project team worked to coordinate with the Western Interstate Commission for Higher Education (WICHE) to meet additional needs that were not otherwise possible to address within the state and continues to learn with this organization and affiliated states in the western region. The team also put together a strategy on how to engage the WY Relocate campaign (Figure 4; a statewide marketing campaign that encourages returning to Wyoming after receiving training or living out of state) as part of their action plan that could serve as a career pathway link to recruit more healthcare workers and their families to Wyoming. Within the Wyoming Department of Health, the Office of Rural Health has various workforce development programs and resources for healthcare professional recruitment, loan repayment programs, and scholarships. Through the Wyoming Health Resources Network, those attempting to join the healthcare workforce in the state can successfully be recruited and placed with doctors and organizations that need professionals.
Rural communities are diverse and have distinctive benefits but also face unique challenges, particularly with regards to the healthcare workforce. Barriers faced by the healthcare workforce are further exacerbated in rural communities given challenges with recruitment, limited resources and because providers cover large geographic areas. Rural communities are often under resourced, making recruiting and retaining the healthcare workforce a challenge. States have approached this challenge in several ways, including by strengthening higher education partnerships and supporting workers in these communities.
Colorado: In June 2022, Colorado Governor Jared Polis signed SB22-172 into law which establishes the Colorado Rural Healthcare Workforce Initiative. This initiative establishes authority for higher education institutions to operate a rural track for any healthcare professional program offered by the institution. In order to receive a scholarship and additional benefits from the track, students must commit to working as a healthcare professional in a rural county for at least two years after completing education and training.
Minnesota: While not developed during the NGA Center’s project, Minnesota operates a successful program for medical students to train and practice in rural communities. Minnesota established the Rural Physician Associate Program (RPAP) at the University of Minnesota School of Medicine in 1971. The RPAP is a nine-month program for University of Minnesota third-year medical students to live and train in rural communities across both Minnesota and western Wisconsin. After more than 50 years of the program, two out of three former students practice in Minnesota, with more than 40 percent practicing in rural locations.
Oregon: The Oregon Office of Rural Health (ORH) has been the coordinating body for rural and frontier health in Oregon since 1979. ORH partnered with Oregon Health & Science University (OHSU) in 1989 to increase its ability to bring statewide resources to rural areas. Supported by the Federal Office of Rural Health Policy (FORHP), the state of Oregon and OHSU, ORH offers assistance to hospitals, clinics and communities to strengthen the rural and frontier health care delivery system.
West Virginia: West Virginia has invested in numerous scholarship and loan repayment programs with in-state service obligations including the West Virginia Rural Scholars Program. This program provides fourth year medical students stipends and advanced admission incentives for students committed to practicing rural or small town family medicine in West Virginia. The Marshall University Rural General Surgery Residency program, beginning in 2023, is the first ever officially designated Rural Track Program in any specialty accredited by the Accreditation Council for Graduate Medical Education. Planning for this program was funded by the West Virginia Higher Education Policy Commission Division of Health Sciences through the Rural Residency Grant Program. Marshall University, one of West Virginia’s public universities, leveraged these funds to obtain federal funding from HRSA. This program will provide surgery residents with half of their training at Logan Regional Medical Center in southern West Virginia. In June 2022, West Virginia Governor Jim Justice announced an initiative to recruit, train and strengthen West Virginia’s EMS workforce. Included in this allocation of $10 million of West Virginia’s CAREs Act funds are investments for mobile ambulance simulators to allow educational opportunity to reach rural and remote parts of the state.
Wyoming: Wyoming is uniquely situated in the United States as it is the least populated state in the country, despite its large geographic size. Because of these factors, Wyoming is considered a highly rural state with a small number of more populated cities and large towns containing larger healthcare systems, specialty care and training programs. Given this, the healthcare workforce planning conducted by the project team focused on rural workforce considerations ranging from increased access to education and clinical training to affordability support programs (e.g., education reimbursement, housing access through the U.S. Department of Agriculture and other mortgage funding programs for healthcare workers) to personal connections that would encourage retention of primary and specialty care providers (including supports to encourage providers’ family members to build their own businesses in the state and using the WY Relocate campaign).
Critical to bolstering a strong nursing workforce is strengthening the nursing pipeline since nurses touch on every aspect of care provision in most healthcare settings. Nurses are the backbone of the healthcare workforce, serving as the throughline of care for patients in care settings. States have developed many creative ways to overcome the nursing shortage, from expanding career pathway entry points to investing in programs that increase the retention of workers.
Connecticut: Through a collaboration between Connecticut State Colleges and Universities (CSCU), the Office of Workforce Strategy (OWS), the Connecticut Hospital Association, the Connecticut Conference of Independent Colleges (CCIC), the University of Connecticut and several state agencies, the state of Connecticut has launched CT Health Horizons, a three-year, postsecondary program designed to address nursing and behavioral health provider shortages. The program will provide tuition support to an anticipated 1,200 students with a focus on students in nursing and social work programs. The $35 million initiative will be overseen by OWS and CSCU.
Colorado: The NGA Center provided technical assistance to the Colorado state team on policy options for nurse licensure, ways to support nursing faculty, nursing education flexibilities and strategies to expand enrollment for nursing programs. With this information, and in an effort to help meet industry demand for bachelor’s prepared nurses and provide upward mobility for current healthcare workers, Colorado Governor Jared Polis signed SB22-003 in April 2022 to expand a nurse training pathway at community colleges. This legislation permits community colleges in the Colorado Community College System and Aims Community College to offer a practical pathway for Licensed Practical Nurses (LPNs) to earn a bachelor’s degree in nursing (BSN). The colleges will leverage existing programs, resources, equipment and faculty to design the pathway and allow students to earn a BSN faster, thereby increasing the pool of trained employees for hospitals to hire from.
Minnesota: Minnesota has seen positive outcomes from their Next Generation Nursing Assistant Initiative, a public-private partnership led by the Minnesota Office of Higher Education Commissioner. The initiative provides participants with free training, books and uniforms in addition to covering the cost of the nursing certification examination. In its first year, the Nursing Assistant Initiative surpassed its service goal of 1,000 students by training over 1,300 certified nursing assistants (CNAs). Because of this success, Minnesota Governor Tim Walz announced a $2.4 million investment to extend the program through February 2023 – an investment made possible by the state’s COVID-19 Management Appropriation Fund.
Recruiting and retaining the direct care workforce remains a challenge for states and territories. These workers provide essential services for older adults, people with disabilities and people undergoing intensive rehabilitation. These workers are also in particularly high demand as the U.S. population continues aging and retiring. While the direct care workforce is essential, these workers are often paid low wages and in short supply. States and territories have been focused on improving wages and recruiting more people to these careers.
Colorado: In recent years, Colorado has set several goals to strengthen its direct care workforce. One aim was to work with employers to achieve better compliance of implementing a $15 per hour base wage for direct care workers. Over 70 percent of employers in the state report that they have implemented this base wage. Colorado also aimed to establish interagency agreements with the community college system, Department of Labor and Employment and the Department of Higher Education; two of three of these agreements are in place. Colorado is also piloting a new standardized curriculum for direct care workers to provide transferable certifications for this group.
Oregon: In February 2022, the NGA Center worked with Oregon to define strategies to support retention of temporary direct care workers post-pandemic. The state was interested in understanding state strategies to transition temporary direct care workers (who qualified to serve as direct care workers under pandemic-related regulatory flexibilities) to qualify as full direct care workers once the flexibilities were removed. Relatedly, Oregon was interested in identifying state strategies to implement career pathways within direct care roles to support retention within the sector. The NGA Center provided a research memo and a presentation on these issues for the Oregon Department of Human Services Aging and People with Disabilities Long Term Care Workforce Roundtable in February 2022. As a result of this technical assistance, Oregon began funding a competency-based CNA apprenticeship model to increase the pipeline for direct care roles in the state. This program is fully operational as of March 2023.
Wisconsin: Wisconsin recently developed policy and budget recommendations with input from the NGA Center and other policy experts to support, recruit and retain the direct care workforce. These included compensation-related recommendations, such as salary, benefits and professional development opportunities. Wisconsin Governor Tony Evers included healthcare workforce initiatives totaling $150 million in his 2023-2025 budget. The state also has a Wisconsin Long Term Care Advisory Council to gather strategies, resources and ideas from the field. Wisconsin also developed a direct care worker certificate program as part of WisCaregiver Careers, a program to provide CNA jobs, training and incentives to people in the state.
There is increasing demand for behavioral health services, but the workforce has not grown to meet these needs. The COVID-19 pandemic has exacerbated mental illness in the U.S., with the Centers for Disease Control finding in its Household Pulse Survey that adults reporting symptoms of anxiety or depression have increased substantially since 2019. For instance, in February 2023, about 28 percent of adults over 18 had anxiety disorder symptoms, 22 percent had depressive disorder symptoms and 32 percent had anxiety or depressive disorder symptoms. Compared to a study in 2019 that found that 8 percent of adults had anxiety disorder symptoms, 7 percent had depressive disorder symptoms and 11 percent had symptoms of anxiety or depressive disorder, it is clear that the need for behavioral services is much greater today than it was a few years ago. States are investing in their behavioral health workforce to address this increased need by removing barriers to entry and supporting career pipelines in this sector, as well as by increasing Medicaid reimbursement rates for these providers.
California: The California Department of Health Care Services manages three grants to support the behavioral healthcare workforce and improve access to care. The Mentored Internship Program supports students aged 18 or older at multiple stages of their career development by providing on-the-job experience for students entering the behavioral health workforce. The Governor’s Office recently announced $17 million in grants for 39 nonprofit providers and tribal organizations to support the next generation of the behavioral healthcare workforce through this program. The Expanding Peer Organization Capacity grant helps organizations build capacity and infrastructure to deliver peer recovery supports for individuals with mental health challenges and substance use disorders. Finally, the Peer Workforce Investment Grant supports peer-run behavioral health programs to build capacity and infrastructure to advance service volume and promote collaboration with other provider types.
Colorado: In 2022, Colorado Governor Jared Polis signed SB22-181 into law, allocating federal stimulus funding to strengthen Colorado’s behavioral health workforce. Colorado’s Behavioral Health Administration (BHA) has developed a plan to use these funds to improve access to care, strengthen the career pipeline and publicly funded behavioral health providers, remove barriers for those entering the field, and reduce administrative burdens that impede people-centered care within the current workforce. Additionally, SB21-137 provides $9 million in federal stimulus funding for the Behavioral Health incentive program. This program provides funding to institutions with degree and certificate programs in behavioral health to grant scholarships to students in rural and frontier counties, as well as enrolled students experiencing adverse circumstances. Workforce specialists at the BHA will focus on recruitment and training opportunities to enhance the diversity of the behavioral healthcare workforce, and they conducted an environmental scan of behavioral healthcare workforce initiatives across state agencies.
Oklahoma: Oklahoma has invested Medicaid dollars in Certified Community Behavioral Health Clinics (CCBHC), both boosting jobs in the field and addressing gaps for vulnerable populations. With the addition of CCBHCs, the state added more than 600 new jobs to the behavioral health workforce, addressing previous gaps in Community Mental Health Centers. In addition to a new range of services, CCBHCs receive an enhanced Medicaid reimbursement rate based on their costs of services to best address the needs of the populations served. Additionally, Oklahoma has developed several career ladders, including a Health Care Eco System Career Ladder. The ladder, designed to connect potential members of the healthcare workforce to an easy-to-use tool for career mapping, outlines entry level, mid-career and advanced occupations for individuals interested in direct patient care. The career ladder includes a section on behavioral health, including professions like social and human service assistants, mental health and substance abuse social workers, and substance abuse and behavioral disorder counselors.
Oregon: Oregon has made significant investments in expanding and diversifying the state’s behavioral health workforce. In 2021, the state invested $80 million in ARPA funds to develop a diverse behavioral health workforce through the Behavioral Health Workforce Initiative. The initiative funded scholarships, loan repayment, retention and peer workforce development in licensed and non-licensed occupations, and made clinical supervision grants providing supervised experience to associates or other individuals to obtain a credential. In May 2022, Oregon distributed one-time grants to 162 behavioral health agencies totaling to $132.66 million for staff compensation and workforce retention and recruitment.
Wyoming: The state has been working on a coordinated approach to behavioral health in recent years. In addition, Wyoming is exploring paraprofessional training programs for mental health and substance use disorder healthcare workers that require less training than traditional providers, which could help fill gaps in access to care provision currently available in the state.
Additionally, Wyoming Governor Mark Gordon’s Health Task Force and the Wyoming Innovations Partnership will focus on prioritizing the healthcare workforce. The task force has identified the behavioral health workforce as a top priority and will be investigating different options for entry level positions to generate interest in the field, which will flow into a career pipeline. Credential stacking and other options are also being investigated to help strengthen the current workforce and meet the evolving needs of communities.
The Next Generation of the Healthcare Workforce project yielded great success in multiple states, creating opportunities for state leaders to address concerns directly related to the healthcare workforce. Through their work together, states have learned ways to strengthen their healthcare career pathways, strategies to attract and retain workers, and methods to coordinate these efforts effectively. While recruitment is important, state teams have noted that they must work together to grow the workforce instead of luring existing workers across state lines. States and territories can coalesce around shared goals while continuing to develop solutions to address their specific workforce challenges.
Given the successful outcomes for states in this project and heightened interest from both state and territorial leaders, the NGA Center announced that the Next Generation of the Healthcare Workforce Project would continue for a second year. The NGA Center combined both the Learning Collaborative and the Knowledge Exchange Network into one large group of 23 states and territories to move forward the conversation on barriers and challenges to supporting the healthcare workforce. During 2023, the NGA Center is expanding the workforce development toolkit for project states and territories and continuing technical assistance on healthcare workforce topics for project states and territories. The NGA Center is also continuing to hold virtual webinars with national experts and will hold in-person regional workshops during the summer of 2023 to support unique challenges faced by the country’s diverse landscape. In August 2023, the NGA Center will also hold a healthcare workforce summit for all project states and territories. The NGA Center is excited to continue this important work and looks forward to supporting state and territorial leaders throughout 2023 and beyond.
The National Governors Association Center for Best Practices (NGA Center) would like to thank the Health Resources and Services Administration (HRSA) in the U.S. Department of Health and Human Services for their generous support in development of this publication under National Forum Cooperative Agreement No. U98OA09028. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of HRSA or the U.S. Department of Health and Human Services.
This paper was developed by Anna Heard, Shelby Hockenberry, Elijah McCabe, Portia Polk, Charlie Schonberger and Amanda Winters of the NGA Center for Best Practices and Hannah Maxey and Courtney Medlock of Veritas Health Solutions. The NGA Center would like to thank the state officials and other experts whose expertise contributed to this publication as well as the NGA staff who contributed expertise and review of this publication.
Heard, A., Hockenberry, S., McCabe, E., Polk, P., Schonberger, C., Winters, A., Maxey, H., Medlock, C. Preparing the Next Generation of the Healthcare Workforce: State Strategies for Recruitment and Retention. Washington, DC: National Governors Association, July 2023.